A 42YR OLD MALE WITH FEVER AND COUGH.
MEDICINE CASE REPORT: PATIENT WITH FEVER AND COUGH
This is an online E log book to discuss our patient's de-identified health data shared after taking his/her/guardian's signed informed consent. Here we discuss individual patient's problems through series of inputs from available global online community of experts with an aim to solve those patient's clinical problems with collective current best evidence based inputs. This e-log book also reflects my patient centered online learning portfolio and your valuable comments on comment box is welcome.I've been given this case to solve in an attempt to understand the topic of "Patient clinical data analysis" to develop my competency in reading and comprehending clinical data including history, clinical findings, investigations and come up with a diagnosis and treatment plan.
CHIEF COMPLAINTS:
A 42 YEAR OLD MALE PATIENT PRESENTED WITH A HISTORY OF
1. FEVER SINCE 8 DAYS AND
2. COUGH SINCE 8 DAYS .
HISTORY OF PRESENTING ILLNESS:
1. ON THE DAY OF ADMISSION(19/05/2021):
Patient was apparently asymptomatic 8 days back when he developed FEVER , which was sudden in onset, intermittent, high grade, not associated with chills and rigor, relieved on medication.
Then, he also developed COUGH, which was productive, with scanty, non blood stained, mucoid, odourless sputum. No diurnal variation, No positional variation. No hemoptysis.
- No complaints of Shortness of breath (SOB), Orthopnea, or PND.
- No complaints of chest pain, pedal edema, decreased urine output, no loss of appetite.
2. ON 20/05/2021:
Patient's FEVER has SUBSIDED and his oxygen saturation was 86% on room air.
Patient has developed SHORTNESS OF BREATH ( GRADE III -- MMRC ). Patient was prescribed O2 inhalation with intermittent BiPAP, and his saturations increased to 90% with 15L of O2.
3. ON 21/05/2021:
Patient is AFEBRILE.
Patient was subjectively feeling better.
Patient has SHORTNESS OF BREATH ( GRADE II -- MMRC). Patient was prescribed O2 inhalation with intermittent BiPAP, and his saturation improved to 95% with 10L of O2.
4. ON 22/05/2021:
Patient is febrile, probable cause being IV infusion of fluids and steroids. It can be INFUSION THROMBOPHLEBITIS.
Patient also developed hyperglycemia, which can be due to use of dexamethasone.
HISTORY OF PAST ILLNESS:
--Patient is a known case of hypertension, since 5yrs.
--Patient has no history of Diabetes Mellitus, tuberculosis, coronary artery disease, epilepsy.
PERSONAL HISTORY:
DIET: mixed
APPETITE: normal
SLEEP: adequate
BOWEL AND BLADDER: regular
ADDICTIONS: no known addictions
ALLERGIES: no allergies
DRUG HISTORY:
Patient was on AMLONG 5mg for Hypertension.
FAMILY HISTORY:
The patient's mother also tested positive for COVID-19.
GENERAL EXAMINATION: Patient was conscious and coherent.
Pallor: absent
Icterus: absent
Clubbing: absent
Cyanosis: absent
Lymphadenopathy: absent
Edema: absent
VITALS:
ON THE DAY OF ADMISSION ( 19/05/2021):
BP: 100/70 mm pf Hg
PR: 110bpm
RR: 30 cycles/ min
TEMP: febrile, 104°F
SpO2: 86% on Room air, 6L OF OXYGEN FOR 96%
ON 20/05/2021:
BP: 110/70 mm Hg
PR: 120 bpm
RR: 30 cycles/min
TEMP: afebrile
SpO2: 86% on room air, 90% with 15L of oxygen
ON 21/05/2021:
BP: 110/70 mm Hg
PR: 110/min
RR: 26/min
TEMP: Afebrile
SpO2: 90% on 10L of oxygen
SYSTEMIC EXAMINATION:
1. CVS: S1 and S2 heard
2. PA: No significant observations
3.CNS: All senses are normal.
INVESTIGATIONS:
ON THE DAY OF ADMISSION (19/05/2021):
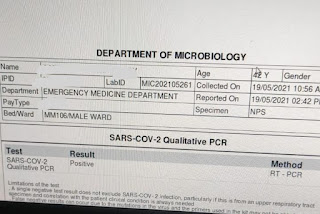
COVID-19 RT-PCR REPORT
SERUM LDH LEVEL
RENAL FUNCTION TEST REPORT
COMPLETE BLOOD PICTURE
LIVER FUNCTION TEST
PLASMA D-DIMER LEVELS
ON 21/05/2021:
CHEST X--RAY :
PROVISIONAL DIAGNOSIS:VIRAL PNEUMONIA SECONDARY TO COVID-19 INFECTION
TREATMENT:
1. On the day of admission ( 19/05/2021 ):
1.PROPPED UP POSTURE
2.OXYGEN INHALATION 6-8lit/day
3.FREQUENT PRONE POSITION
4.INJ. DEXA 8mg iv/OD
5.INJ. CLEXANE 40mg SC OD
6.T. PCM 650mg / PO/ TID
7.Strict temperature charting 4th hourly
8.SYP ASCORIL
9.TAB AMLONG 5mg / OD
10. NEBULISATION BUDOCORT & DUOLIN
11. TAB. LIMCEE PO/OD
12.TAB. ZINCOVIT PO/OD
2. TREATMENT ON 20/05/2021:
1. INTERMITTENT BIPAP
2. INJ. DEXA 8mg IV
3. INJ. CLEXANE 40mg SC
4. Tab. PCM 650mg/ PO/ QID
5. Tab. LIMCEE
6. Tab. ZINCOVIT PO/OD
7. Tab. AMLONG 5mg/OD
3. TREATMENT ON 21/05/2021:
1. INTERMITTENT BIPAP
2. AWAKE PRONING
3. INJ. DEXA 8mg IV
4. INJ. CLEXANE 40mg SC
5. Tab. PCM 650mG /PO/QID
6. Tab. LIMCEE
7. Tab. ZINCOVIT PO/OD
8. Tab. AMLONG 5mg/OD
9. MAINTAIN HYDRATION

















Comments
Post a Comment